Jesse Benet and Deb Srebnik, King County Behavioral Health and Recovery Division
In 2014, the Washington State Legislature passed SB 6312, which mandated that each regional service area of the state must provide mental health services, chemical dependency services, and medical care services to Medicaid clients under a fully integrated managed care health system, by 2020. On the tailwind of this bill, King County, Washington, launched several health and human services transformation initiatives.
In 2013, the Familiar Faces Initiative had begun taking a data-driven, LEAN cross-sector approach to understanding individuals who repeatedly cycled through our jails. These individuals, known to us as our “familiar faces,” represent a population with complex health issues—and 94% of them have a behavioral health issue too. The availability of unprecedented data-matching between institutions serving these individuals in King County sent us on a journey of current-state mapping and future-state visioning, resulting in a new approach and discipline that drives and informs all adult Diversion and Reentry Services programs implemented and administered by the county.
Data in Data-Driven Justice
To develop data-driven responses by more fully understanding the needs of the high-utilizer population, King County substantially enhanced its cross-sector data sharing and analysis capabilities.
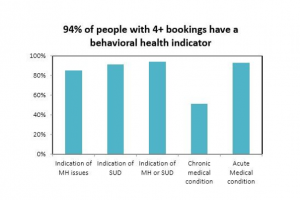 For nearly 20 years, the county’s Department of Adult and Juvenile Detention (DAJD) had been transmitting daily jail booking and release data to the Behavioral Health and Recovery Division (BHRD). As the administrator for publicly funded behavioral health services in the county, BHRD used this data to provide contracted behavioral health agencies with daily “alerts” about clients who had been booked into jail so that agencies could provide transitional care and reentry services. Building on this foundation, BHRD developed a data-sharing agreement with the county’s public health department, which administers the Jail Health Services (JHS). Analysis of JHS diagnoses, BHRD behavioral health service data, and jail bookings revealed that 94 percent of people with 4 or more bookings in a year have an indicator of a mental or substance use issue.
For nearly 20 years, the county’s Department of Adult and Juvenile Detention (DAJD) had been transmitting daily jail booking and release data to the Behavioral Health and Recovery Division (BHRD). As the administrator for publicly funded behavioral health services in the county, BHRD used this data to provide contracted behavioral health agencies with daily “alerts” about clients who had been booked into jail so that agencies could provide transitional care and reentry services. Building on this foundation, BHRD developed a data-sharing agreement with the county’s public health department, which administers the Jail Health Services (JHS). Analysis of JHS diagnoses, BHRD behavioral health service data, and jail bookings revealed that 94 percent of people with 4 or more bookings in a year have an indicator of a mental or substance use issue.
This population of people frequently detained in jail, many of whom had mental or substance use issue indicators, were coined “familiar faces.” Nearly all familiar faces (93 percent) had at least 1 acute medical condition, and about half (51 percent) had at least 1 chronic medical condition. More than half were experiencing homelessness at booking.
Interest among stakeholders in these initial findings and enthusiasm for their potential to shape solutions led to additional data sharing agreements to obtain information on municipal jail bookings, mental health and drug court involvement, emergency medical services (EMS) responses, Healthcare for the Homeless Network services, prior juvenile justice involvement, and Medicaid hospital and emergency department utilization.
 From this additional data, we learned among other things that familiar faces were more likely to be male and non-white than the overall jail population, and less than 8 percent had opted into an adult therapeutic court within the City of Seattle or King County.
From this additional data, we learned among other things that familiar faces were more likely to be male and non-white than the overall jail population, and less than 8 percent had opted into an adult therapeutic court within the City of Seattle or King County.
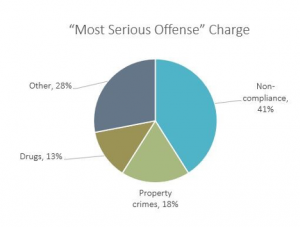
EMS contact, which occurred among 38 percent of the population in question, was related to behavioral health issues at a much higher rate (39 percent) than for the overall population of people using EMS (12 percent). Noncompliance charges were the most common reason for incarceration, and about half (49 percent) had had juvenile justice system involvement. Using these results, the county’s budget office conducted an influential cost analysis that showed that, under existing practices, a familiar face accounted for at least $28k per year in county-administered services alone, largely within the criminal legal system. The 2016 cost analysis is available here.
Mapping, Learning, and Centering on the Consumer
Many social conditions contribute to the systems that churn individuals through institutional and crisis-oriented responses that create familiar faces. The goal of the Familiar Faces Initiative was to gain better outcomes for high utilizers of the jail who have physical and behavioral health challenges. The vision for the Familiar Faces Initiative centered on the individual’s ability to readily access any health and social service supports needed, facilitated by a nimble and responsive care team that can address the level of care and specific needs of the individual, regardless of payer. This vision was developed collectively with cross-sector partners to achieve the following outcomes:
- Improved health status
- Improved housing stability
- Reduced criminal justice involvement
- Reduced avoidable hospital emergency department use
The intent was to transform systems to make health and human services the standard response to familiar faces, rather than the previously prevailing criminal justice system default. This work required examining the many existing systems and approaches to the complex social problems facing individuals with behavioral health conditions, many of whom are experiencing homelessness and lack access to the resources needed to meet basic needs. The transformation required is summarized by these systems change efforts currently underway:
- Diversion becomes a guiding principle and focus: Crisis diversion facilities, Law Enforcement Assisted Diversion (LEAD), and other outreach resources are available to first responders and to familiar faces.
- Jails, court, and hospitals become institutions of last resort.
- Services are grounded in harm reduction and trauma-informed, person-first care.
 The Familiar Faces Initiative has given way to new approaches to serving a population with highly complex needs. Early implementation of some core aspects of the Future State Vision are underway, including a demonstration of a Flexible Care Management Team approach. Though similar to forensic assertive community treatment, and loosely based on the assertive community treatment core principles, the Flexible Care Management Team program has some key differences, including a prosecutorial liaison, rather than a clinician criminal justice specialist. We look forward to sharing insights and providing updates as the work progresses.
The Familiar Faces Initiative has given way to new approaches to serving a population with highly complex needs. Early implementation of some core aspects of the Future State Vision are underway, including a demonstration of a Flexible Care Management Team approach. Though similar to forensic assertive community treatment, and loosely based on the assertive community treatment core principles, the Flexible Care Management Team program has some key differences, including a prosecutorial liaison, rather than a clinician criminal justice specialist. We look forward to sharing insights and providing updates as the work progresses.
Like what you’ve read? Sign up to receive the monthly GAINS eNews!


